26 ways to avoid getting sick this winter
Come on, it's not the end of the world.

1. Take Your Fight-amins
Your vitamin D levels may run on E in winter. That matters: D can spur your body to fight off colds. In fact, taking 10,000 IU of vitamin D3 a week may cut your risk of upper respiratory infection in half, say Canadian researchers.
2. Stop Touching Yourself
Unless sterile surgical gloves are part of your winter wardrobe, keep your mitts off your mug. People who occasionally touch their eyes and nose are 41 percent more likely to develop frequent upper respiratory infections than hands-off folks, a 2013 study in the Journal of Occupational Health found. And if you think hand sanitizer is the answer, we refer you to #17.
3. Say Hello to Yogurt
Cold and flu viruses might have an Achilles' heel: Greek yogurt. In a study published in Clinical Nutrition, people who consumed a specific strain of probiotics daily reduced their risk of catching one of these bugs by 27 percent. Aim to eat at least one serving a day of a Greek yogurt with live cultures, suggests Spencer Payne, M.D., an associate professor of rhinology at the University of Virginia School of Medicine.
4. Refill Your Meditation
We'd like you to contemplate perfect health. Researchers from the University of Wisconsin at Madison found that people who meditated took 76 percent fewer sick days than those who were not so zen. Meditating trains you to stay focused and calm, which helps alleviate stress that can leave you vulnerable to infection. To get started, try the brief mindfulness sessions available for free at marc.ucla.edu.
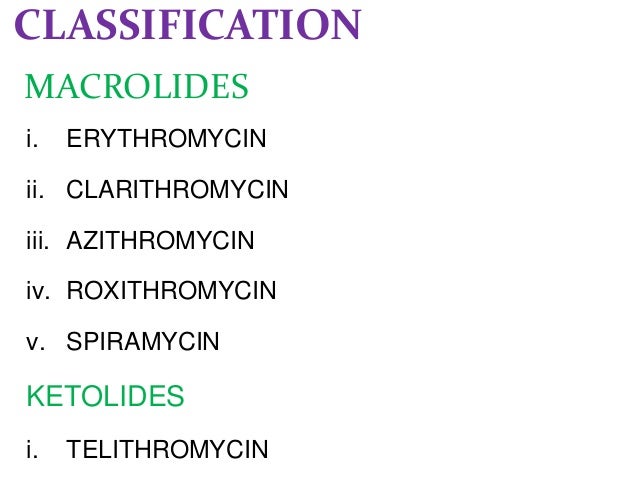
5. Nail Your Tea Shot
Skip the black coffee and brew some green tea. Its magic ingredient, a catechin called epigallocatechin gallate (EGCG), can damage influenza virus particles and stop them from entering your system, a German study reveals. The scientists believe this kick-ass catechin may also interfere with pneumonia-causing bacteria. Knock back as much green tea as you want, or take a daily EGCG supplement, say study authors Joerg Steinmann, M.D., and Eike Steinmann, Ph.D. Try the Now Foods 400-milligram tablets.
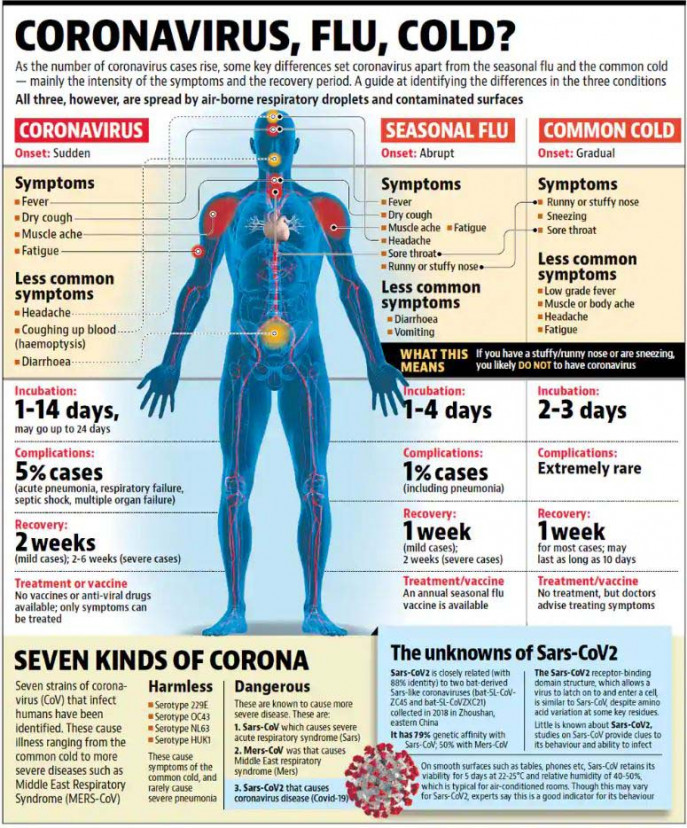
6. Order a Shot
"The number one thing you can do to prevent the flu is get vaccinated," says Bill Schaffner, M.D., a professor of preventive medicine at Vanderbilt University. Even if another strain infects you, the shot may reduce symptoms.
7. Train on Time
Hit the gym before your jab. When you exercise prior to receiving a flu shot, the post-exercise inflammation boosts your body's immune response to the virus in the vaccine, according to a study review in Brain, Behavior, and Immunity. That translates to more powerful infection protection. How much sweat is enough? A British study found that people who performed 25 minutes of lifts targeting their biceps and deltoids were able to increase their immune response.
8. Start Nasal Maneuvers
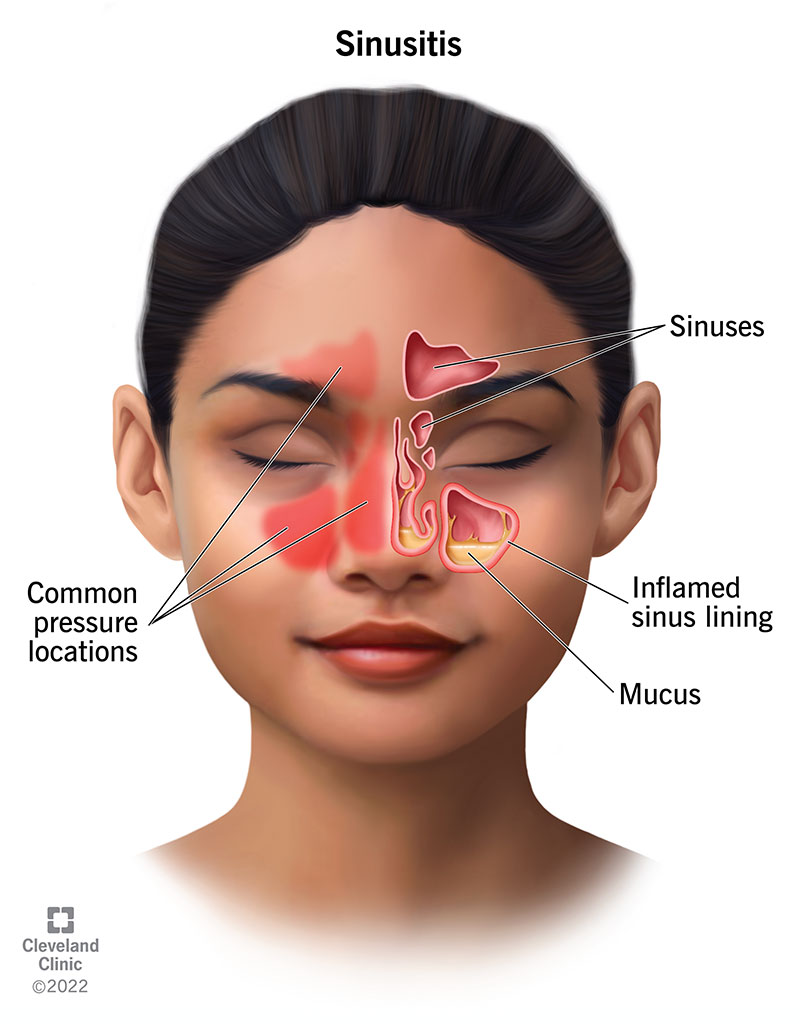
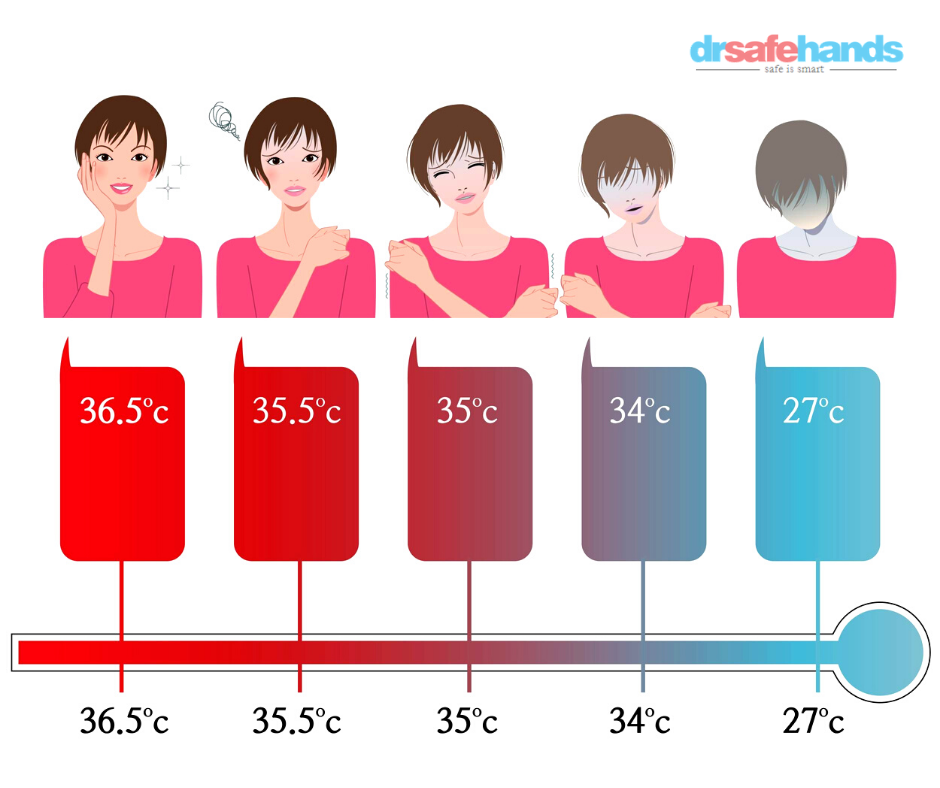
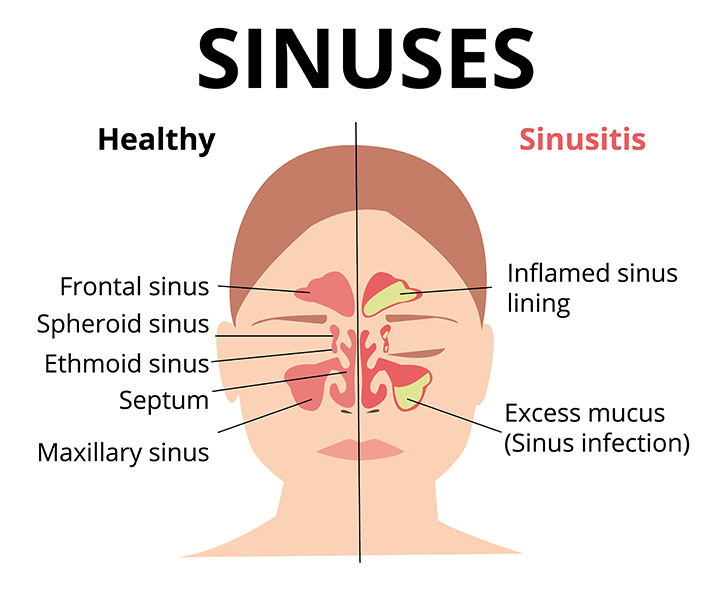
Freezing your butt off? Worry more about your nose. The cilia in your nasal and sinus cavities sweep away illness-causing pathogens, but the rate at which the cilia move is affected by temperature, says James Palmer, M.D., director of the division of rhinology at the University of Pennsylvania. "When cilia are warmed up, they beat a little faster, and when it's cold they beat more slowly. So spending a lot of time in the cold may make it easier for you to get sick." That is, unless you breathe through a scarf.
9. Boil Over
Viruses that cause foodborne illnesses tend to loiter on produce. So to further slash your chance of sickness, try blanching your greens--kale, spinach, and chard, for example--in boiling water for two to three minutes. Then dunk them into ice water to stop the cooking. (Blanching can give your greens a different kind of flavor.) Heating to 212°F greatly reduces norovirus in spinach, a study in the Journal of Food Protection reports.
10. Refuse the Booze
UMass Medical School research suggests that one binge-drinking session triggers a flood of cytokines, proteins that can induce fever and increase inflammation. Any more than five drinks in two hours is a binge, the CDC says.
11. Break Your Dry Spell
It isn't enough just to keep your nose cozy (#8)--there's a moisture mandate too. If your nasal passages are dried out, their natural antimicrobial properties will suffer, says Dr. Payne. "Try to keep the humidity level in your home between 30 and 50 percent." When you're at work, spritz your schnoz three or four times a day with a saline gel or spray like Ayr Saline Nasal Mist ($3, drugstore.com).
12. Sweat Out a Cold
Moderate exercise is nothing to sneeze at. In fact, it can slash your risk of catching a cold by 27 percent, Korean researchers report. Working out switches on your immune response, possibly by sending a cascade of "natural killer cells" to hunt the rhinovirus. Already ill? Keep exercising, Dr. Schaffner advises. "Exercise stimulates the production of epinephrine, which constricts blood vessels in and around your mucous membranes and can relieve nasal discomfort."
13. Teach Yourself to Fish
Note that we said "moderate" exercise in #12: Strenuous workouts can leave you vulnerable to infection. But if you want to keep up the intensity, at least fill your plate with fish. A 2012 study in Brain, Behavior, and Immunity found that increasing your omega-3 intake can spur postexercise production of infection-fighting cells, which can help protect against certain infections. Tired of tuna melts? Top your pizza with anchovies.
14. Say "Hum Bug!"
Humming may annoy other people a bit, but it really annoys germs. "Humming has been shown to increase nitric oxide in the nose, which is antimicrobial," says Dr. Payne.
Try this technique from an Indian study: Take a deep breath, close one nostril, and exhale out the other nostril as you hum. Repeat on the other side. Do this five times. Allergy sufferers who tried it after using a steroid nasal spray twice a day for three months felt about half as congested as those who only used a spray, the study reports.
15. Arrest a Hacker
Menthol always gets the cough-quelling props, but where's the love for eucalyptus? A study in the aptly named journal Cough reports that cineole, a compound found in eucalyptus, can help ease your cough symptoms, possibly by reducing inflammation and helping the bronchi in your lungs expand, increasing airflow as a result. When people suffering from acute bronchitis took 200 milligrams of cineole before each meal, their symptoms improved 22 percent more than a placebo group's did. Try SinuCare soft gels, which contain cineole.
16. Steep Gingerly
Swallow some ginger for what ails you. Researchers in Taiwan have discovered that fresh ginger can inhibit respiratory syncytial virus from attaching to cells and may even reduce its ability to replicate. So what in the world is respiratory syncytial virus? Just a bug that in severe cases can lead to bronchiolitis or pneumonia. Grate some ginger in hot water for a spicy tea, or add it to your next stir-fry with vegetables and garlic.
17. Wash Your Hands of It
It takes a good scrub with soap and water to actually rub a virus off your skin, Dr. Payne says. That means 20 seconds at the sink and a thorough drying: Wet hands are more likely to spread germs than dry ones, notes the CDC.
18. Go to the Mat
Pretzels for immunity? Scientists in Japan speculate that twisting yourself into yoga stretches may help boost your immune defenses, which in turn can better prepare you to fight illnesses like pneumonia, colds, and the flu. The combo of relaxation and physical activity triggers an increase in saliva levels of beta-defensin 2, an antimicrobial peptide that breaks down invading microbes. Just one 90-minute yoga session doubles beta-defensin 2.
19. Carry a Loaded Gum
Freshen your breath and stop bugs in their tracks. Past research shows that xylitol, a sweetener in some chewing gums, can prevent Streptococcus pneumoniae from establishing a stronghold in your body. And now a review from Turkey concludes that xylitol can reduce your risk of ear and sinus infections. Try Ice Breakers Ice Cubes, which contain 1,200 milligrams per piece.
20. Cover Your Wiener
Sauerkraut may provide sweet relief. Researchers in Italy report that Lactobacillus plantarum, a type of probiotic found in such fermented foods as kraut and kimchi, may reduce the potency of a certain kind of strep bacteria. The L. plantarum triggers a protein that helps control inflammation while simultaneously slowing bacterial growth. Give your sandwiches and hot dogs a kick by layering on King's Kimchi or Gold Mine's Organic Raw Sauerkraut.
21. Hibernate for Health
A shuteye deficit can be a nightmare for your immune system: According to a 2013 study conducted in Finland, a single workweek of less than four hours of sleep a night can alter the way your genes function, changing pathways that switch on your immune response and potentially increasing inflammation. For a better night's rest, consider changing up your bedroom lighting with a bulb that can help you reach dreamland faster.
22. Don't Smoke
Time to take a permanent cigarette break. Lighting up leaves your body vulnerable to the flu, say Korean researchers. Smoking raises a person's odds of catching the H1N1 bug, a.k.a. swine flu, more than fivefold.
23. Breathe Easier
Not a smoker? Good. Now don't hang around with anyone who is. Scientists in India report that when people breathe in even a small amount of smoke, their nasal cilia need more than double the time to clear particles, compared with people who haven't been exposed to secondhand smoke--which can increase vulnerability to respiratory infections.
24. Embrace Your Honey
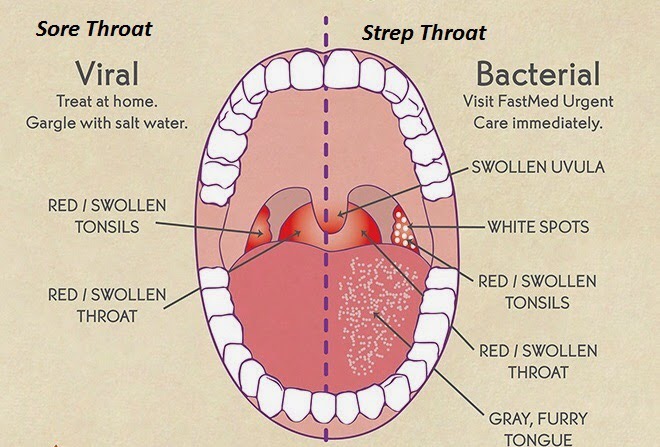
That green tea we recommended (#5)? Here's your sweetener. A study in the journal Microbiology found that when colonies of Streptococcus pyogenes--the strep throat bug--were treated with manuka honey, the bacteria count fell by up to 85 percent. And a 2014 study from Pakistan found that the sticky stuff may also inhibit forms of staph, pneumonia, and salmonella.
25. Heat Smart
Does green tea make you gag? Think ginger (#16) is genuinely disgusting? We don't care what you brew, as long as you down something hot. People who drank a piping hot (165°F) beverage felt rapid improvement in more of their cold and flu symptoms than those who downed fluids at room temperature, according to a study published in the journal Rhinology.
26. Boost Your Herb Appeal
Adding rosemary to a dish means you're also sprinkling in an antiviral ingredient: carnosic acid. This compound helps shield your body from respiratory syncytial virus (see #16) by interfering with its ability to infect its ability to infect a host and replicate, a Korean study found. Shake the herb over roast chicken.
Reference: today.com/health/26-ways-avoid-getting-sick-winter-1d80290214






:max_bytes(150000):strip_icc():format(webp)/GettyImages-170510625-ab389eae92cf426fbb4bd3d2f7299323.jpg)






















:max_bytes(150000):strip_icc():format(webp)/coughing-156415712-resized-56a2f5805f9b58b7d0cfdf87.jpg)





 6-
6- 
 وبلاگ تخصصی سلامت شامل مجموعه مطالب پزشکی است و اطلاعات مفیدی در رابطه با بهداشت، ایمنی، سلامتی بدن و راه های پیشگیری از بیماریها را در اختیار شما کاربر محترم می گزارد.
وبلاگ تخصصی سلامت شامل مجموعه مطالب پزشکی است و اطلاعات مفیدی در رابطه با بهداشت، ایمنی، سلامتی بدن و راه های پیشگیری از بیماریها را در اختیار شما کاربر محترم می گزارد.